Pericoronitis
Pericoronitis, a dental condition often overshadowed by its more well-known counterparts like cavities or gum disease, presents a unique set of challenges and discomforts for those affected.
This inflammatory condition occurs when the gum tissue around the wisdom teeth, or any tooth partially breaking through the gum, becomes infected and swollen, leading to pain, difficulty in chewing, and in severe cases, a significant infection that can affect overall health.
In this article, we delve into the causes, symptoms, and treatment options for pericoronitis, aiming to shed light on this condition that can disrupt daily life and oral health.
Table of Contents
What is Pericoronitis?
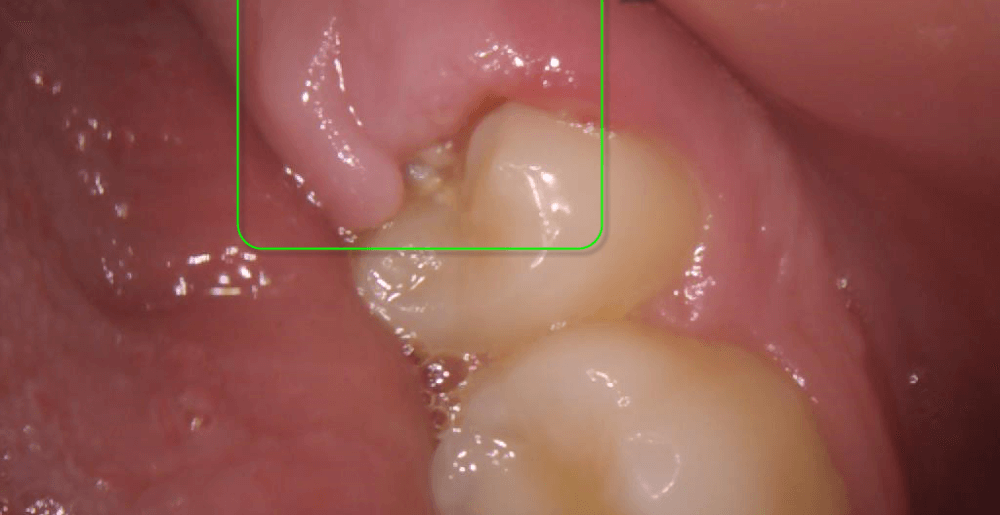
Pericoronitis is a dental condition characterized by the inflammation of the gum tissue surrounding a partially erupted tooth, most commonly seen around the wisdom teeth (third molars).
This inflammation can occur when a wisdom tooth does not fully emerge into the mouth, leading to the formation of a gum flap (operculum) over the tooth.
Food particles and bacteria can get trapped under this flap, causing an infection and swelling of the surrounding gum tissue.
Read more: Gum Flap Over Wisdom Tooth
Symptoms of Pericoronitis
The symptoms of pericoronitis can vary from mild discomfort to severe pain and infection, depending on the extent of inflammation and whether the condition is acute or chronic.
Common symptoms include:
- Pain and Tenderness: The area around the affected tooth can be painful and tender to touch, often worsening with biting or pressure.
- Swelling: The gum tissue around the emerging tooth may appear swollen and red.
- Difficulty Opening the Mouth (Trismus): In severe cases, the inflammation can lead to difficulty in opening the mouth fully.
- Bad Taste or Odor: Accumulation of food particles and bacteria under the gum flap can lead to a foul taste or bad breath.
- Pus Discharge: In cases of infection, pus may be present around the affected area, contributing to the bad taste and odor.
- Fever: A systemic infection can lead to fever and a general feeling of unwellness.
- Swollen Lymph Nodes: The lymph nodes under the jaw or in the neck may become swollen and tender due to the infection.
What causes Pericoronitis?
Pericoronitis is primarily caused by the partial eruption of a wisdom tooth, which can create a flap of gum tissue (operculum) over the tooth. This partial eruption provides an ideal environment for bacteria to thrive, leading to several contributing factors:
- Trapped Food and Bacteria: The gum flap can trap food particles, plaque, and bacteria, making it difficult to clean the area effectively with regular brushing and flossing. This accumulation of debris and bacteria can lead to infection and inflammation of the surrounding gum tissue.
- Poor Oral Hygiene: Inadequate oral hygiene can exacerbate the buildup of plaque and bacteria around a partially erupted wisdom tooth, increasing the risk of pericoronitis.
- Mechanical Irritation: The gum flap over the partially erupted tooth can be irritated by chewing or biting, which can further inflame the area and contribute to the development of pericoronitis.
- Crowding: Wisdom teeth often struggle to find enough space to emerge properly in the mouth, leading to partial eruptions. Crowded teeth can make it even harder to maintain good oral hygiene around the wisdom tooth, increasing the risk of pericoronitis.
- Stress: While not a direct cause, stress is believed to affect the body’s immune response, potentially making the mouth more susceptible to infections like pericoronitis.
Pericoronitis risk factors
Pericoronitis risk factors are conditions or behaviors that increase the likelihood of developing inflammation around a partially erupted wisdom tooth.
Key risk factors include:
- Age: Pericoronitis most commonly affects young adults in their late teens to mid-20s, coinciding with the age range when wisdom teeth typically erupt.
- Poor Oral Hygiene: Inadequate brushing and flossing can lead to the accumulation of food particles and bacteria around the partially erupted tooth, increasing the risk of infection.
- Wisdom Teeth Eruption: The process of wisdom teeth trying to break through the gums (eruption) is a direct risk factor for pericoronitis, especially if the teeth are impacted or partially erupted, creating a flap of gum tissue that can trap debris and bacteria.
- Crowded Teeth: Individuals with crowded teeth may be more susceptible to pericoronitis because crowded conditions make it harder to maintain good oral hygiene around the wisdom teeth, leading to increased plaque and bacteria buildup.
- Tobacco Use: Smoking or using other tobacco products can impair the mouth’s ability to fight off infection and heal, thereby increasing the risk of pericoronitis.
- Stress: High levels of stress can weaken the immune system, making it harder for the body to combat infections, including those in the mouth.
- Poor Nutrition: A diet lacking in essential nutrients can compromise the body’s immune response, potentially increasing susceptibility to infections like pericoronitis.
- Previous Episodes: Individuals who have previously experienced pericoronitis may be at a higher risk of developing the condition again, especially if the underlying causes, such as a partially erupted wisdom tooth, have not been addressed.
How does Pericoronitis affect my oral health?
Pericoronitis can significantly impact your oral health in several ways, especially if left untreated.
Here are some of the ways pericoronitis can affect your oral health:
- Infection and Abscess Formation: One of the primary concerns with pericoronitis is the risk of infection, which can lead to the formation of an abscess. An abscess is a pocket of pus that forms due to the infection, and it can cause severe pain and swelling. If the infection spreads beyond the initial area, it can lead to more serious health issues.
- Gum Disease: The inflammation associated with pericoronitis can contribute to the development or exacerbation of gum disease (periodontal disease) around the affected tooth and neighboring teeth. Gum disease can lead to gum recession, bone loss, and eventually tooth loss if not properly managed.
- Tooth Decay: The difficulty in cleaning the area around a partially erupted wisdom tooth can lead to an increased risk of tooth decay. Food particles and bacteria can easily become trapped under the gum flap, creating an environment conducive to decay not only of the wisdom tooth but also of adjacent teeth.
- Spread of Infection: If the infection associated with pericoronitis is not treated, it can spread to other parts of the mouth, the jaw, and even to distant parts of the body through the bloodstream, a condition known as sepsis, which is life-threatening.
- Difficulty Eating and Speaking: The pain and swelling caused by pericoronitis can make it uncomfortable or even painful to eat, chew, or speak, which can impact your daily life and nutritional intake.
- Impact on Overall Health: Emerging research suggests a link between oral health issues, including infections like pericoronitis, and broader health concerns such as cardiovascular disease, diabetes, and respiratory infections. This connection highlights the importance of maintaining good oral hygiene and addressing dental issues promptly.
Pericoronitis Treatment
Pericoronitis treatment varies depending on the severity of the condition. The primary goal is to reduce inflammation, treat the infection, and alleviate pain.
Here are the common approaches to treating pericoronitis:
Mild Pericoronitis
For cases where the infection is mild and localized:
- Oral hygiene: Improved oral hygiene can help manage and prevent pericoronitis. This includes thorough brushing, flossing, and possibly using a water flosser to remove food particles and bacteria trapped under the gum flap.
- Warm salt water rinses: Rinsing the mouth with warm salt water several times a day can reduce swelling and discomfort.
- Antibacterial mouthwash: Using an antibacterial mouthwash prescribed by a dentist can help reduce the bacterial load in the affected area.
Moderate to Severe Pericoronitis
In more severe cases, additional treatments may be necessary:
- Antibiotics: If the infection spreads beyond the gums or the patient exhibits systemic symptoms like fever, antibiotics may be prescribed to combat the infection.
- Pain relief: Over-the-counter pain relievers such as ibuprofen can help manage pain and reduce inflammation. In some cases, stronger pain medication may be prescribed.
- Professional cleaning: A dentist or dental hygienist might need to clean the area thoroughly to remove debris and bacteria from under the gum flap.
Surgical Options
If pericoronitis recurs frequently or is particularly severe:
- Operculectomy: This minor surgical procedure involves removing the gum flap (operculum) that covers the partially erupted tooth. This can prevent the accumulation of food particles and bacteria.
- Tooth Extraction: In cases where pericoronitis is recurrent and severe, or if the wisdom tooth is impacted and causing other dental issues, extraction of the affected tooth may be recommended.
Ongoing Management
- Regular dental check-ups: Regular visits to the dentist can help monitor the condition and prevent future episodes of pericoronitis.
- Good oral hygiene practices: Continuing with good oral hygiene practices is crucial to prevent the recurrence of pericoronitis and maintain overall oral health.
FAQ on Pericoronitis
Will pericoronitis go away on its own?
Pericoronitis may temporarily subside on its own, especially if it’s mild and triggered by a specific irritant that has been removed. Without addressing the underlying issue, such as improving oral hygiene around the affected tooth or seeking dental treatment, the condition often recurs and can become more severe. In cases where the tooth is partially erupted and continues to trap food and bacteria, professional dental care is usually necessary to fully resolve the issue and prevent future episodes.
How do I know if I have pericoronitis?
If you’re experiencing swelling and redness in the gums around a tooth that hasn’t fully emerged, often a wisdom tooth, accompanied by pain or discomfort in the area that might extend to the jaw or ear, you could be dealing with pericoronitis. This condition can also make it challenging to open your mouth or swallow and might be characterized by a bad taste in your mouth or foul breath. In some cases, you might even have a fever or feel generally unwell. These signs, particularly around a wisdom tooth, suggest it’s important to see a dentist for proper diagnosis and treatment.
What are the early stages of pericoronitis?
The early stages of pericoronitis typically involve mild symptoms localized around the affected tooth, often a wisdom tooth. These symptoms can include:
– Minor pain or discomfort in the area where the tooth is erupting
– Slight swelling and redness of the gum tissue around the partially erupted tooth
– A bad taste in the mouth or bad breath caused by the infection
– Difficulty biting or chewing without discomfort
What happens if pericoronitis is left untreated?
If pericoronitis is left untreated, the infection can spread to the surrounding tissues, leading to more severe swelling, pain, and potentially leading to a systemic infection that affects other parts of the body. In extreme cases, it can result in a serious condition called Ludwig’s angina, which is a life-threatening infection of the floor of the mouth. Untreated pericoronitis can also lead to tooth decay, gum disease, and the loss of the affected tooth.
Can I prevent pericoronitis?
Yes, pericoronitis can often be prevented with good oral hygiene practices, including regular brushing, flossing, and using antiseptic mouthwash to reduce bacteria buildup. Regular dental check-ups allow for early detection and management of potential issues with wisdom teeth or other partially erupted teeth. In some cases, preemptive removal of wisdom teeth that are at risk of causing pericoronitis may be recommended by a dentist or oral surgeon.
Fact Checked
Our dedicated team rigorously evaluates every article and guide to ensure the information is factual, up-to-date, and free of bias.
Updated Regularly
We update our articles and reviews regularly to ensure you have access to the latest data in the dental industry.
The content on Dental3DU’s blog is intended for educational purposes only. This information should not be relied upon as professional medical counsel. Be sure to always consult with your dentist about the dangers and benefits of any medication, treatment or procedure.







