Mandibular Tori: Causes, Symptoms & Removal

Mandibular tori (singular: torus) are bony growths that develop on the mandible, or lower jaw, specifically along the surface nearest to the tongue. These growths are typically benign (non-cancerous) and vary in size.
They can appear on one or both sides of the jaw and are known as torus mandibularis when referring to the condition. The plural form, used when referring to both sides, is mandibular tori.
Key takeaways
- Bony growths: Mandibular tori are harmless bumps on the inner jawbone, usually near the midline and below the premolar teeth.
- Common: They are relatively common, affecting about 6-8% of the population in the US, but prevalence varies between ethnicities.
- Causes: The exact cause is unknown, but it likely involves a combination of genetics, environmental factors (like teeth clenching), and possibly diet.
- Symptoms: Usually asymptomatic (no symptoms), but large tori can make oral hygiene difficult or cause discomfort, pain, or interfere with dentures.
- Treatment: Typically not required. Surgery is only considered if tori cause problems. Read more: Mandibular tori removal
Not related to cancer: Mandibular tori are benign and not cancerous. However, any unusual mouth changes should be checked by a dentist to rule out oral cancer. Read more: Early Stage Mandibular Tori Cancer
Vitamins and minerals: While not directly linked to tori development, sufficient intake of calcium, vitamin D, and other essential nutrients is crucial for overall bone health.
Table of Contents
What exactly are Mandibular Tori
Mandibular tori, or torus mandibularis, are harmless bony growths that develop on the inner surface of the lower jawbone, typically near the midline and below the premolar teeth. They appear as smooth, painless bumps that are usually symmetrical, meaning they occur on both sides of the jaw.
hey are relatively common, affecting about 6-8% of the population in the United States, but the prevalence varies significantly between ethnic groups. They are more common in Asians, Inuit populations, and people of Polynesian descent.
Mandibular Tori causes
The exact cause of mandibular tori is not fully understood, but research suggests a combination of genetic, environmental, and possibly nutritional factors contribute to their development.
Here’s a closer look at these potential causes:
Genetic predisposition
- Heredity: There appears to be a genetic component to mandibular tori, as they are more common in certain families and ethnic groups. This suggests that genetic predisposition plays a significant role in their development. Having family members with MT significantly increases your risk, suggesting a strong genetic component.
Environmental factors
- Mechanical Stress: Chronic mechanical stress on the jaw, such as from teeth clenching, may stimulate bone growth, leading to the formation of tori. The theory is that the jawbone responds to increased stress with additional bone growth as a form of adaptation.
- Dental Occlusion: Abnormalities in the way teeth come together (occlusion) might also contribute to the formation of tori by creating uneven forces on the jawbone.
- Bruxism (teeth grinding): Habitual teeth grinding or clenching can put stress on the jawbone, possibly stimulating bone growth and leading to MT formation.
- Bone density: People with higher bone density or changes in bone density may be more prone to developing MT.
- Age: MT are more commonly diagnosed in adults over 40, although they can develop at any age.
Nutritional factors
- Diet: Some studies have suggested a link between diet and the development of mandibular tori. For example, diets high in certain nutrients, like omega-3 fatty acids found in fish, have been associated with a higher prevalence of tori. The theory is that certain diets may influence bone metabolism and growth.
- Vitamin deficiencies: Some studies suggest deficiencies in vitamins like A, C, and D might be linked to MT development, although more research is needed.
- Calcium: High calcium intake through diet or supplements might be a contributing factor, though evidence is inconclusive.
Other considerations
- Sex: MT are slightly more common in females than males.
- Ethnicity: Certain ethnic groups, like Asians, Inuit populations, and Polynesians, have a higher prevalence of MT.
Note that while these factors can contribute to the development of mandibular tori, their presence does not necessarily mean a person will develop tori.
Many individuals with one or more risk factors never develop mandibular tori, indicating that the process is complex and not fully understood.
Want to find out more? What Causes A Bump On The Roof Of Mouth?
Dental Tori symptoms
Mandibular tori are usually asymptomatic, meaning they often do not cause any noticeable symptoms or discomfort. However, their presence can be identified by certain characteristics and, in some cases, they may lead to issues that require attention. Here are the main aspects related to the symptoms and potential concerns associated with mandibular tori:
Identification and characteristics
- Location: Mandibular tori are bony growths located on the inner side of the lower jaw, near the tongue, and can vary in size.
- Shape and Size: They can appear as small nodules or large lumps, and their size can increase gradually over time. They may be symmetrical on both sides of the jaw or present only on one side.
- Texture: The overlying mucosa (gum tissue) is usually normal in appearance, and the tori themselves are hard to the touch, being composed of bone.
Potential issues and symptoms
While mandibular tori are generally not problematic, certain conditions or situations may arise where they become noticeable or cause discomfort:
- Oral Hygiene Difficulty: Large tori can make it challenging to clean certain areas of the mouth effectively, potentially leading to oral hygiene issues.
- Discomfort or Pain: If the tori are particularly large, they might cause discomfort during eating, speaking, or other oral activities. They can also be susceptible to trauma or ulceration from food, dental appliances, or during dental procedures.
- Interference with Dental Work: Mandibular tori can complicate dental procedures, including the fitting of dentures, crowns, or bridges. They may require modification of dental appliances or even surgical removal to accommodate these devices properly.
- Speech Impediment: In rare cases, very large tori might affect speech by restricting the movement of the tongue or altering the flow of air during speech.
When to seek help
Although mandibular tori are benign and often require no treatment, you should consult with a dentist or oral surgeon if:
- You experience discomfort, pain, or difficulty with oral functions due to the tori.
- The tori interfere with the fit or comfort of dental appliances.
- You have concerns about oral hygiene or the appearance of the tori.
In such cases, a professional can assess the need for potential treatment options, including monitoring, improving oral hygiene practices around the tori, or surgical removal if they cause significant issues.
Mandibular Tori treatment
Treatment for mandibular tori is typically considered only when they cause discomfort, interfere with oral functions, or complicate dental procedures.
In many cases, mandibular tori do not require any treatment due to their benign nature and the lack of symptoms.
When intervention is necessary, the primary treatment option is surgical removal. Here’s an overview of considerations and procedures related to the treatment of mandibular tori:
When is treatment necessary?
- Discomfort or Pain: If the tori cause significant discomfort or pain during eating, speaking, or other activities.
- Interference with Oral Hygiene: When their size or location makes it difficult to maintain proper oral hygiene, leading to recurrent oral health issues.
- Complications with Dental Procedures: If the tori obstruct the fitting or wearing of dentures, or interfere with other dental work such as crowns, bridges, or implants.
- Trauma and Ulceration: Frequent trauma or ulceration on the tori due to their size or location may also necessitate removal.
Surgical removal
- Procedure: The surgical removal of mandibular tori involves making an incision in the gum tissue over the growths, exposing the bone, and then carefully removing the tori using surgical instruments. The goal is to smooth the bone surface to prevent regrowth and to improve comfort and function.
- Anesthesia: The procedure is typically performed under local anesthesia, but sedation options may be available for patients with anxiety or for more extensive cases.
- Recovery: Post-operative recovery may involve mild to moderate discomfort, which can usually be managed with over-the-counter or prescription pain relievers. Patients are advised to follow a soft diet and maintain good oral hygiene to promote healing. The recovery period varies but generally involves several days to a week of reduced activity to allow for initial healing.
- Risks and Complications: As with any surgical procedure, there are risks of infection, bleeding, or nerve damage, although these are relatively rare. Proper surgical technique and post-operative care minimize these risks.
Non-Surgical management
In cases where surgical removal is not necessary or desired, management focuses on monitoring the tori for changes in size or symptoms and addressing any specific issues they cause, such as adjusting dental hygiene practices or modifying dental appliances to accommodate the tori.
Mandibular Tori removal
Mandibular tori removal is a surgical procedure aimed at eliminating bony growths on the inner side of the lower jaw. This procedure is typically considered when tori cause discomfort, interfere with oral functions, or complicate the fitting and wearing of dental appliances.
Here’s a detailed look at the process, recovery, and considerations associated with mandibular tori removal:
Indications for removal
- Discomfort or Pain: Significant discomfort or pain during eating, speaking, or other activities.
- Interference with Oral Hygiene: Difficulty in maintaining proper oral hygiene due to the size or location of the tori.
- Dental Procedure Complications: Obstruction in the fitting or wearing of dentures, or interference with other dental work.
- Frequent Trauma or Ulceration: If the tori are frequently traumatized or ulcerated by food, dental appliances, or during dental procedures.
Surgical procedure
- Pre-operative Assessment: Includes a thorough examination, possibly with X-rays or CT scans, to understand the size and structure of the tori.
- Anesthesia: The procedure is usually performed under local anesthesia, but sedation or general anesthesia may be used depending on the complexity of the case and patient preference.
- Incision and Removal: The surgeon makes an incision in the gum tissue over the tori to expose the bone. Specialized dental instruments are then used to carefully remove the bony growths. The goal is to smooth the underlying bone to prevent regrowth and to minimize post-operative discomfort.
- Closure: The gum tissue is sutured back into place over the bone.
Recovery and aftercare
- Pain Management: Patients may experience mild to moderate pain after the anesthesia wears off, which can typically be managed with prescribed or over-the-counter pain relievers.
- Diet: A soft or liquid diet is recommended for the first few days to a week after surgery to allow the surgical site to heal.
- Oral Hygiene: Gentle oral hygiene practices are important to prevent infection. Patients may be advised to use a special mouthwash or saltwater rinses to keep the area clean.
- Follow-up: A follow-up visit is usually scheduled to ensure proper healing and to remove sutures if they are not self-dissolving.
Risks and complications
As with any surgical procedure, there are potential risks, including infection, bleeding, or temporary numbness due to nerve disturbance. Serious complications are rare, and the procedure has a high success rate when performed by an experienced oral surgeon.
What to have in mind
- Necessity: Removal is only recommended when the tori cause significant issues, as they are otherwise benign.
- Regrowth: While not common, there is a possibility of tori regrowing after removal, especially if the underlying causes (like bruxism) are not addressed.
Read more: Mandibular Tori removal.
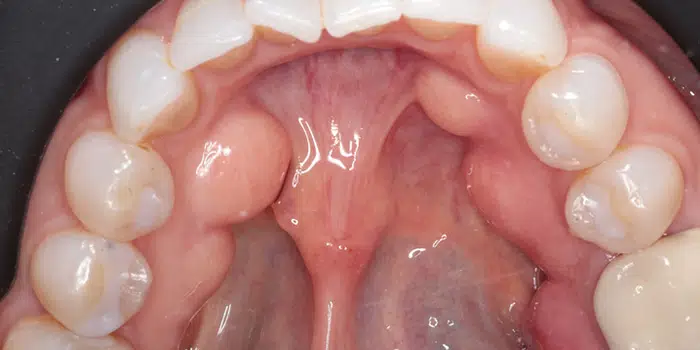
Mandibular Tori pictures


Mandibular Tori cancer
Mandibular tori are benign and are not associated with cancer. These growths are considered a normal anatomical variation rather than a pathological condition.
The development of mandibular tori is typically linked to genetic factors, environmental influences such as mechanical stress on the jaw (e.g., from teeth grinding), or possibly dietary factors, but not to malignant transformation.
Any significant changes in the mouth, such as the sudden appearance of growths, changes in existing growths, or the development of ulcers that do not heal, should be evaluated by a healthcare professional.
While mandibular tori themselves are not cancerous, it’s important to distinguish them from other types of growths or lesions in the mouth that may require further investigation to rule out malignancy.
Oral cancers can develop in any part of the mouth, including the lips, tongue, cheeks, floor of the mouth, hard and soft palate, sinuses, and throat, and can be serious if not diagnosed and treated early.
Symptoms of oral cancer may include persistent sores, lumps or thickening tissues in the mouth, difficulty swallowing, and changes in the fit of dentures.
If there’s any concern about a growth in the mouth or changes to existing mandibular tori, you should consult with a dentist or an oral and maxillofacial surgeon.
Early stage Mandibular Tori cancer
Mandibular tori are benign bony growths on the mandible (lower jaw) and, by definition, are not cancerous and do not become cancerous. The term “Mandibular Tori cancer” is a misnomer because mandibular tori themselves do not undergo malignant transformation or represent an early stage of cancer.
Still, it’s important to differentiate between mandibular tori and other oral lesions or growths that could potentially be malignant.
Oral cancer can manifest in various ways, including lumps, ulcers, or changes in the oral tissues that do not heal. These signs can occur anywhere in the mouth, including areas where mandibular tori are typically found.
Recognizing Oral Cancer
Early detection of oral cancer significantly improves the prognosis. Here are some signs and symptoms associated with oral cancer that should prompt immediate evaluation by a healthcare professional:
- A sore or lesion in the mouth that does not heal within two weeks.
- A lump or thickening in the cheek.
- A white or red patch on the gums, tongue, tonsil, or lining of the mouth.
- Difficulty chewing or swallowing.
- Difficulty moving the jaw or tongue.
- Numbness of the tongue or other areas of the mouth.
- Swelling of the jaw that causes dentures to fit poorly or become uncomfortable.
- Unexplained weight loss.
- Persistent bad breath.
Evaluation and Diagnosis
If there’s a concern about a possible malignancy in the mouth, a thorough evaluation by a dentist or a specialist in oral and maxillofacial surgery is necessary. This evaluation may include:
- Visual Examination: Checking for lesions, lumps, or irregular tissue changes in the mouth.
- Palpation: Feeling the inside of the mouth and the neck for lumps or enlarged lymph nodes.
- Biopsy: Taking a small sample of tissue from a suspicious area for laboratory analysis to determine if cancer cells are present.
- Imaging Tests: X-rays, CT scans, MRI, or PET scans may be used to assess the extent of the disease and to help with staging if cancer is found.
In Conclusion
While mandibular tori are not related to cancer, any unusual changes in the mouth should be evaluated promptly. Early diagnosis and treatment of oral cancer can lead to better outcomes. Maintaining regular dental check-ups can help in the early detection of oral health issues, including the early signs of oral cancer. Find out more: Early Stage Mandibular Tori Cancer
Mandibular Tori vitamin deficiency
Mandibular tori, the benign bony growths that develop along the inner surface of the lower jaw, are not typically associated with vitamin deficiencies.
Their formation is believed to be influenced more by genetic factors, mechanical stresses (such as teeth grinding or clenching), and possibly other environmental factors rather than nutritional deficiencies.
You need to nderstand that overall bone health, including the health of the jawbone, can be affected by nutritional status, including the intake of certain vitamins and minerals:
Vitamins and Minerals Important for Bone Health
- Calcium: Essential for bone formation and maintenance. A deficiency in calcium can lead to weakened bone structure and density.
- Vitamin D: Helps the body absorb calcium and is crucial for bone health. Vitamin D deficiency can lead to bone softening diseases such as osteomalacia in adults and rickets in children.
- Phosphorus: Works with calcium to build strong bones and teeth.
- Vitamin K: Plays a role in bone metabolism and helps the body make proteins for healthy bones.
- Magnesium: Important for bone formation and influences the activities of osteoblasts and osteoclasts, the cells responsible for the formation and resorption of bone.
While there’s no direct link between vitamin deficiencies and the development of mandibular tori, maintaining a balanced diet rich in these vitamins and minerals is essential for overall bone health and may indirectly influence conditions related to bone density and growth.
Find out more: Mandibular Tori Vitamin Deficiency
FAQ on Mandibular Tori
How do I know if I have Mandibular Tori?
To determine if you have Mandibular Tori, look for hard, bony growths along the inner side of your lower jaw, near the tongue. These growths are usually painless and vary in size. However, the most reliable way to confirm their presence is through a dental examination. A dentist can visually inspect and feel the area for tori and may use X-rays to assess their size and density. If you suspect you have Mandibular Tori, consult with a dental professional for an accurate diagnosis.
What is mandibular tori caused by?
Mandibular tori are primarily caused by a mix of genetic predisposition and environmental factors, including mechanical stress on the jaw from habits like teeth grinding or clenching. Dietary influences, such as a high intake of certain nutrients like omega-3 fatty acids, have been suggested to play a role in their development. The exact cause is not fully understood, but it’s believed that these factors together contribute to the formation of these benign bony growths along the inner side of the lower jaw.
Can mandibular tori go away?
Mandibular tori do not typically go away on their own. These benign bony growths on the inner side of the lower jaw tend to remain once formed or may gradually grow larger over time. In cases where they cause discomfort or interfere with oral functions, surgical removal is an option.
How do you get rid of Mandibular Tori naturally?
There is no natural method to eliminate Mandibular Tori once they have formed. These benign bony growths on the jawbone are permanent unless surgically removed. While maintaining good oral hygiene and managing factors like teeth grinding may help prevent their growth from worsening, the only way to physically remove Mandibular Tori is through a surgical procedure performed by a dental professional.
Is mandibular tori caused by stress?
Mandibular tori are not directly caused by stress in the psychological sense, but mechanical stress on the jaw, such as from teeth grinding or clenching, can contribute to their development. These habits exert extra pressure on the jawbone, potentially stimulating the growth of these benign bony protrusions.
How common is Mandibular Tori?
Mandibular tori are relatively common, affecting a significant portion of the population. The prevalence varies widely among different ethnic groups and geographical regions, with some studies suggesting that up to 10% or more of individuals may have mandibular tori. Their occurrence is influenced by genetic factors and environmental conditions, making them more prevalent in certain families and populations.
Resources
- Mermod M, Hoarau R. Mandibular tori (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4527908/). CMAJ. 2015 Aug 11;187(11):826.
- Radiopaedia.org. Mandibular torus (https://radiopaedia.org/articles/mandibular-torus-2?lang=us).
Fact Checked
Our dedicated team rigorously evaluates every article and guide to ensure the information is factual, up-to-date, and free of bias.
Updated Regularly
We update our articles and reviews regularly to ensure you have access to the latest data in the dental industry.
The content on Dental3DU’s blog is intended for educational purposes only. This information should not be relied upon as professional medical counsel. Be sure to always consult with your dentist about the dangers and benefits of any medication, treatment or procedure.







