
Newsletter Subscribe
Enter your email address below and subscribe to our newsletter

Enter your email address below and subscribe to our newsletter

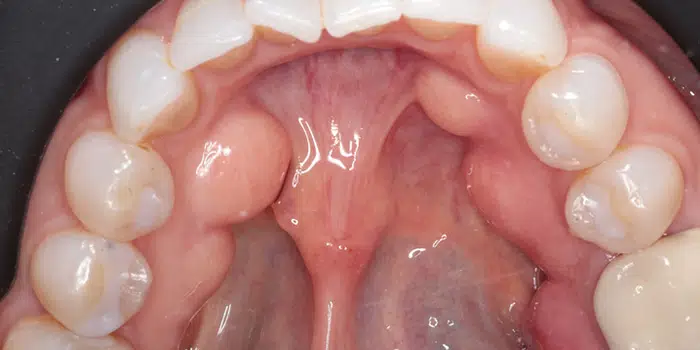
Got bumps under your tongue? Don't panic! They might just be Mandibular Tori, harmless bony growths on your lower jaw. Learn all about symptoms, causes, treatment options, and more. Discover if they're a concern and how to manage them effectively.
Mandibular tori (singular: torus) are bony growths that develop on the mandible, or lower jaw, specifically along the surface nearest to the tongue. These growths are typically benign (non-cancerous) and vary in size.
They can appear on one or both sides of the jaw and are known as torus mandibularis when referring to the condition. The plural form, used when referring to both sides, is mandibular tori.
Key takeaways
Not related to cancer: Mandibular tori are benign and not cancerous. However, any unusual mouth changes should be checked by a dentist to rule out oral cancer. Read more: Early Stage Mandibular Tori Cancer
Vitamins and minerals: While not directly linked to tori development, sufficient intake of calcium, vitamin D, and other essential nutrients is crucial for overall bone health.
Mandibular tori, or torus mandibularis, are harmless bony growths that develop on the inner surface of the lower jawbone, typically near the midline and below the premolar teeth. They appear as smooth, painless bumps that are usually symmetrical, meaning they occur on both sides of the jaw.
hey are relatively common, affecting about 6-8% of the population in the United States, but the prevalence varies significantly between ethnic groups. They are more common in Asians, Inuit populations, and people of Polynesian descent.
The exact cause of mandibular tori is not fully understood, but research suggests a combination of genetic, environmental, and possibly nutritional factors contribute to their development.
Here’s a closer look at these potential causes:
Note that while these factors can contribute to the development of mandibular tori, their presence does not necessarily mean a person will develop tori.
Many individuals with one or more risk factors never develop mandibular tori, indicating that the process is complex and not fully understood.
Want to find out more? What Causes A Bump On The Roof Of Mouth?
Mandibular tori are usually asymptomatic, meaning they often do not cause any noticeable symptoms or discomfort. However, their presence can be identified by certain characteristics and, in some cases, they may lead to issues that require attention. Here are the main aspects related to the symptoms and potential concerns associated with mandibular tori:
While mandibular tori are generally not problematic, certain conditions or situations may arise where they become noticeable or cause discomfort:
Although mandibular tori are benign and often require no treatment, you should consult with a dentist or oral surgeon if:
In such cases, a professional can assess the need for potential treatment options, including monitoring, improving oral hygiene practices around the tori, or surgical removal if they cause significant issues.
Treatment for mandibular tori is typically considered only when they cause discomfort, interfere with oral functions, or complicate dental procedures.
In many cases, mandibular tori do not require any treatment due to their benign nature and the lack of symptoms.
When intervention is necessary, the primary treatment option is surgical removal. Here’s an overview of considerations and procedures related to the treatment of mandibular tori:
In cases where surgical removal is not necessary or desired, management focuses on monitoring the tori for changes in size or symptoms and addressing any specific issues they cause, such as adjusting dental hygiene practices or modifying dental appliances to accommodate the tori.
Mandibular tori removal is a surgical procedure aimed at eliminating bony growths on the inner side of the lower jaw. This procedure is typically considered when tori cause discomfort, interfere with oral functions, or complicate the fitting and wearing of dental appliances.
Here’s a detailed look at the process, recovery, and considerations associated with mandibular tori removal:
As with any surgical procedure, there are potential risks, including infection, bleeding, or temporary numbness due to nerve disturbance. Serious complications are rare, and the procedure has a high success rate when performed by an experienced oral surgeon.
Read more: Mandibular Tori removal.


Mandibular tori are benign and are not associated with cancer. These growths are considered a normal anatomical variation rather than a pathological condition.
The development of mandibular tori is typically linked to genetic factors, environmental influences such as mechanical stress on the jaw (e.g., from teeth grinding), or possibly dietary factors, but not to malignant transformation.
Any significant changes in the mouth, such as the sudden appearance of growths, changes in existing growths, or the development of ulcers that do not heal, should be evaluated by a healthcare professional.
While mandibular tori themselves are not cancerous, it’s important to distinguish them from other types of growths or lesions in the mouth that may require further investigation to rule out malignancy.
Oral cancers can develop in any part of the mouth, including the lips, tongue, cheeks, floor of the mouth, hard and soft palate, sinuses, and throat, and can be serious if not diagnosed and treated early.
Symptoms of oral cancer may include persistent sores, lumps or thickening tissues in the mouth, difficulty swallowing, and changes in the fit of dentures.
If there’s any concern about a growth in the mouth or changes to existing mandibular tori, you should consult with a dentist or an oral and maxillofacial surgeon.
Mandibular tori are benign bony growths on the mandible (lower jaw) and, by definition, are not cancerous and do not become cancerous. The term “Mandibular Tori cancer” is a misnomer because mandibular tori themselves do not undergo malignant transformation or represent an early stage of cancer.
Still, it’s important to differentiate between mandibular tori and other oral lesions or growths that could potentially be malignant.
Oral cancer can manifest in various ways, including lumps, ulcers, or changes in the oral tissues that do not heal. These signs can occur anywhere in the mouth, including areas where mandibular tori are typically found.
Early detection of oral cancer significantly improves the prognosis. Here are some signs and symptoms associated with oral cancer that should prompt immediate evaluation by a healthcare professional:
If there’s a concern about a possible malignancy in the mouth, a thorough evaluation by a dentist or a specialist in oral and maxillofacial surgery is necessary. This evaluation may include:
While mandibular tori are not related to cancer, any unusual changes in the mouth should be evaluated promptly. Early diagnosis and treatment of oral cancer can lead to better outcomes. Maintaining regular dental check-ups can help in the early detection of oral health issues, including the early signs of oral cancer. Find out more: Early Stage Mandibular Tori Cancer
Mandibular tori, the benign bony growths that develop along the inner surface of the lower jaw, are not typically associated with vitamin deficiencies.
Their formation is believed to be influenced more by genetic factors, mechanical stresses (such as teeth grinding or clenching), and possibly other environmental factors rather than nutritional deficiencies.
You need to nderstand that overall bone health, including the health of the jawbone, can be affected by nutritional status, including the intake of certain vitamins and minerals:
While there’s no direct link between vitamin deficiencies and the development of mandibular tori, maintaining a balanced diet rich in these vitamins and minerals is essential for overall bone health and may indirectly influence conditions related to bone density and growth.
Find out more: Mandibular Tori Vitamin Deficiency
To determine if you have Mandibular Tori, look for hard, bony growths along the inner side of your lower jaw, near the tongue. These growths are usually painless and vary in size. However, the most reliable way to confirm their presence is through a dental examination. A dentist can visually inspect and feel the area for tori and may use X-rays to assess their size and density. If you suspect you have Mandibular Tori, consult with a dental professional for an accurate diagnosis.
Mandibular tori are primarily caused by a mix of genetic predisposition and environmental factors, including mechanical stress on the jaw from habits like teeth grinding or clenching. Dietary influences, such as a high intake of certain nutrients like omega-3 fatty acids, have been suggested to play a role in their development. The exact cause is not fully understood, but it’s believed that these factors together contribute to the formation of these benign bony growths along the inner side of the lower jaw.
Mandibular tori do not typically go away on their own. These benign bony growths on the inner side of the lower jaw tend to remain once formed or may gradually grow larger over time. In cases where they cause discomfort or interfere with oral functions, surgical removal is an option.
There is no natural method to eliminate Mandibular Tori once they have formed. These benign bony growths on the jawbone are permanent unless surgically removed. While maintaining good oral hygiene and managing factors like teeth grinding may help prevent their growth from worsening, the only way to physically remove Mandibular Tori is through a surgical procedure performed by a dental professional.
Mandibular tori are not directly caused by stress in the psychological sense, but mechanical stress on the jaw, such as from teeth grinding or clenching, can contribute to their development. These habits exert extra pressure on the jawbone, potentially stimulating the growth of these benign bony protrusions.
Mandibular tori are relatively common, affecting a significant portion of the population. The prevalence varies widely among different ethnic groups and geographical regions, with some studies suggesting that up to 10% or more of individuals may have mandibular tori. Their occurrence is influenced by genetic factors and environmental conditions, making them more prevalent in certain families and populations.
Fact Checked
Our dedicated team rigorously evaluates every article and guide to ensure the information is factual, up-to-date, and free of bias.
Updated Regularly
We update our articles and reviews regularly to ensure you have access to the latest data in the dental industry.
The content on Dental3DU’s blog is intended for educational purposes only. This information should not be relied upon as professional medical counsel. Be sure to always consult with your dentist about the dangers and benefits of any medication, treatment or procedure.
Dental articles in your inbox. Subscribe